The most recent report from Office of the National Coordinator for Health Information Technology (ONC) on hospital interoperability shows 55% of all hospitals can now send, receive, find, and integrate patient information from outside sources into their Electronic Health Records (EHRs). This is an important milestone on the road to robust data exchange.
Much as it is vital to speak the same language as someone else you are speaking with, it is equally important that EHR systems be able to communicate with each other using standardized vocabulary that can easily be interpreted. This ensures that patient data stays accurate, decreases the amount of time spent searching for paperwork during patient appointments, and even creates better health care outcomes.
The government’s push for Health Information Exchanges (HIEs) began in 2009 with the passage of the Health Information Technology for Economic and Clinical Health Act (HITECH). At the time, the focus for health systems centered around EHR adoption rather than interoperability. Today, the market is nearly saturated, with the ONC reporting that 86% of office-based physicians use an EHR.
Challenges
Disparate Data Sources
Despite widespread EHR adoption, there is a distinct lack of interoperability between systems. The biggest roadblocks to interoperability are rooted in fundamental issues in healthcare that have yet to be adequately addressed.
EHRs contain data from a wide range of sources, amongst which there is no standard format for data. Over time, as a record grows in number of providers, contributing EHR systems, and data sources, the data becomes increasingly unwieldy. Recent years have seen a dramatic uptick in use of patient technology such as wearables and mobile apps for tracking health and wellness. Each of these represents a new data source and potentially unique data format.
Lack of standardized terminology
With so many EHRs available, the lack of standardization of terminology and functionality is a major hurdle to interoperability. There are a few primary EHR vendors in the market, health care organizations must choose the EHR that best meets their specific requirements for functionality, implementation, or budget. Not every type of EHR will work for every provider. The pursuit of EHR interoperability remains vital to improving patient care and outcomes, enhancing the workplace environment for providers, and reducing costs.
Each of the EHRs in the market will have unique technical specifications, clinical terminologies, and customizations that prevent the direct sharing of data between systems. Interoperability ensures that patient data can be shared accurately between various systems and entities, which improves communication and facilitates more efficient delivery of patient care.
Looking Ahead
Unarguably, the question is what comes next? What challenges will persist as we look ahead in the years to come? What trends will take hold? What are the key tools and strategies we can use to achieve more widespread EHR interoperability and data exchange?
-
Data Overload and the Need for EHR Interoperability
Most EHRs available today generate tremendous amounts of data, while lacking the necessary tools for data analytics and integration. Expand the number of providers, systems, and data sources, and the record quickly becomes a collection of disparate low-quality data.
A general rule of thumb in analytics is that more data typically yields better insights. However, without the right tools, ever-increasing volumes of complex data will quickly become impossible to navigate. A cursory search on the internet demonstrates the veritable smorgasbord of analytics tools with machine learning capabilities that can easily extract targeted insights from terabytes of data.
EHR interoperability is needed to make them meaningful—for example, translating results into actionable recommendations that trigger workflows in the EHR. The single most critical function of EHRs is the ability to communicate data to others that need it. If the system is not interoperable, this benefit is lost entirely.
The good news is that expanding the capabilities of your EHR to achieve interoperability does not have to be painful. With a wealth of technical expertise and hands-on experience, an expert EHR software provider will build a solution that aligns with your organization’s needs, meets industry standards for interoperability, and can be easily adapted to evolving business needs and industry requirements.
-
Finding Patient Information is (Finally) Getting Easier
Health information exchanges (HIEs) are essential to connect entities and ensure availability of patient medical records. While interoperability remains a major concern for HIE implementation, HIE connectivity is becoming more prevalent across the country.
In March 2020, ONC released the next phase of the 21st Century Cures Act, the interoperability rule, which primarily focuses on blocking of interoperability and patient information. The goal of this phase is to increase transparency and drive patient access to sharing electronic health data, allowing individuals to more easily and effectively coordinate their own healthcare. A recent report reveals meaningful progress for interoperability, with 67% of provider organizations reported they often or nearly always had access to needed records in 2020, up from 28% in 2017. Providers noted improvements in functionality and usability for tasks such as locating and viewing records.
-
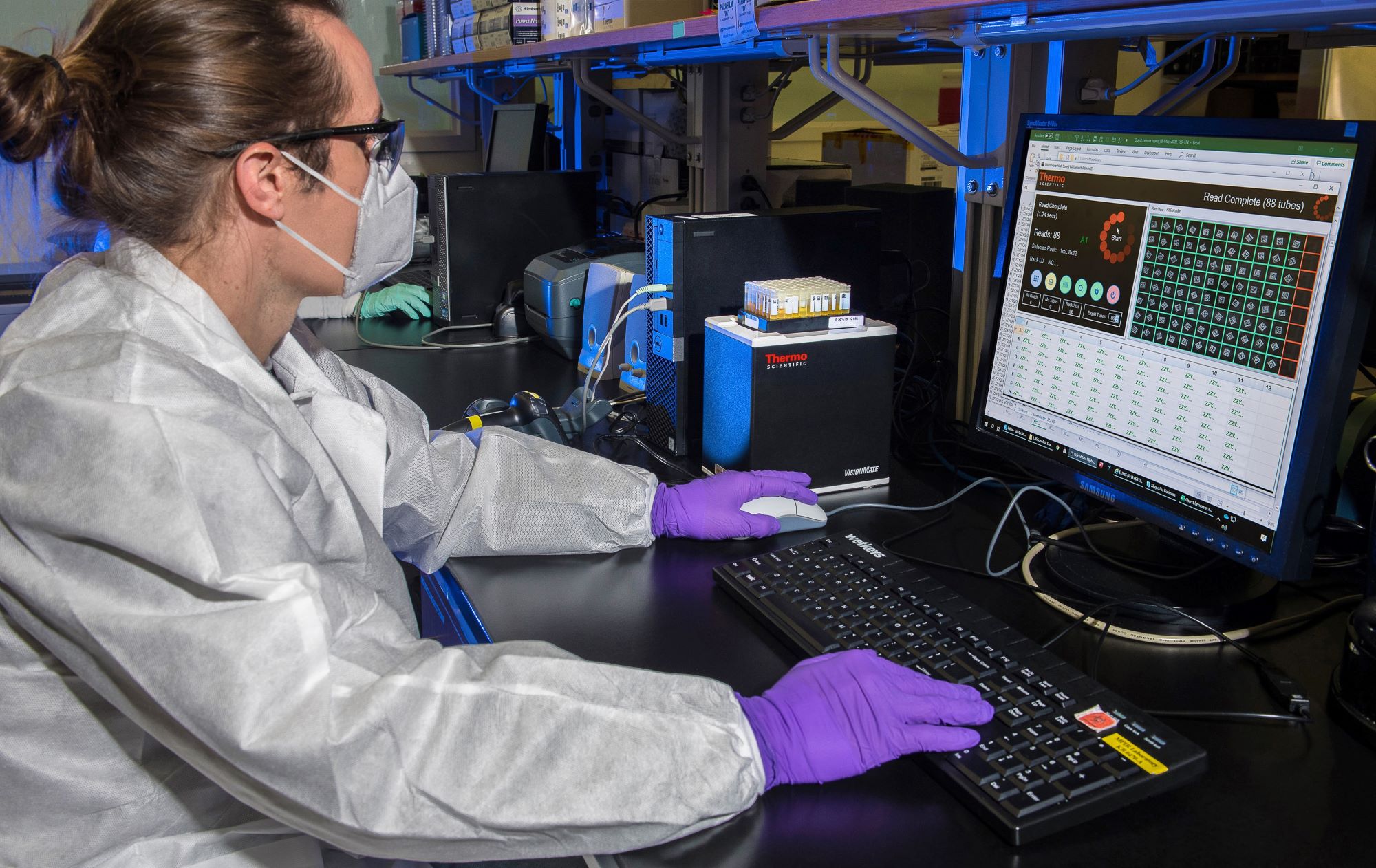
Preparing for a Crisis: Innovation, Infrastructure, Interoperability
2020 was a pivotal year on the path to making digital healthcare a permanent reality. What appeared to have been a coordinated and seamless response to crisis in real time, in fact, reflects years of challenging work and planning. Industry stakeholders and digital innovators have been designing, building, and implementing systems and infrastructure to support a growing digital industry segment.
Covid-19 has underscored the importance of interoperability to this digital infrastructure. The ability to quickly access patient information, exchange data, and make critical, data-driven decisions in real-time provide the agility needed to respond quickly and act decisively.
In an industry already shifting toward increased transparency and data sharing, the pandemic and vaccine rollout have given motivation and momentum to the push for interoperability. In our latest ZipRadio podcast, a panel of seasoned HealthTech experts discuss the persisting challenges to interoperability, expected impacts of Covid-19 on recent efforts, and interoperability solution innovations.